Pulse Oximeters: What They Are, How to Use Them, and What Your Oxygen Level Means
7 min read

Related Topics
Blood sats—hospital jargon for “blood oxygen saturation”—show how much oxygen (O2) currently is circulating in a person’s blood. This helps doctors make informed decisions about their care.
Blood oxygen saturation is a useful measure outside the hospital, too. In fact, there are many good reasons to check your own oxygen level at home. And that’s where a pulse oximeter comes in.
Continue reading to learn why, when, and how to use this handy device
What is oxygen saturation?
Your blood oxygen saturation (often shortened to “oxygen level” or “O2 saturation”) shows the amount of oxygen your red blood cells are carrying. In some very specific instances, a health care provider will use an arterial blood gas (ABG) test to check oxygen levels. More commonly, they (or you) will use a pulse oximeter. In both instances, results are shown as a percentage.
Why is O2 saturation important?
Every organ and every system in your body needs oxygen in order to perform.
When you breathe in, oxygen from the air moves through your lungs and into your arteries. From there, hemoglobin (a protein molecule in your blood) carries it to all of your other cells. These cells use oxygen to create the energy they need to carry out essential functions—including digestion, metabolism, circulation, thinking, and more.
Blood oxygen saturation is one measure of how well your respiratory (breathing) system is working and how efficiently your blood carries oxygen.
What is a normal blood oxygen level?
The normal range for most adults is 95%–100% at sea level.1 At higher elevations, where oxygen in the air is thinner, this range might be slightly lower.
If you’re sick with pneumonia, RSV, or COVID—or have a condition affecting your lungs like chronic obstructive pulmonary disease (COPD) or emphysema—your readings also might be lower.1 Your doctor can help you determine what baseline percentage is normal and healthy for you.
What are the symptoms of low blood oxygen levels?
The medical term for a low blood oxygen level is “hypoxia.”
Sometimes, there are no symptoms. This is especially true if you have mild hypoxia, defined as an O2 saturation between 90%–94%.2 (While abnormal, oxygen levels in this range usually aren’t harmful).2
When hypoxia is mild to moderate (80%–89%), symptoms can include:2,3
- Feeling like you can’t catch your breath
- Feeling like your heart is racing
- Having a headache
- Being overly tired or physically fatigued
- Feeling confused
- Being uncoordinated
- Feeling lightheaded or weak
- Having a bluish tint under your fingernails or on your lips
More severe hypoxia (below 80%) has more severe symptoms, including loss of consciousness, coma, and even death.2 It may be reassuring to know that usually, people don’t suffer from severe hypoxia in isolation. Other conditions or emergencies, like carbon dioxide poisoning, heart failure, or pulmonary edema (fluid filling the lungs), generally cause it.
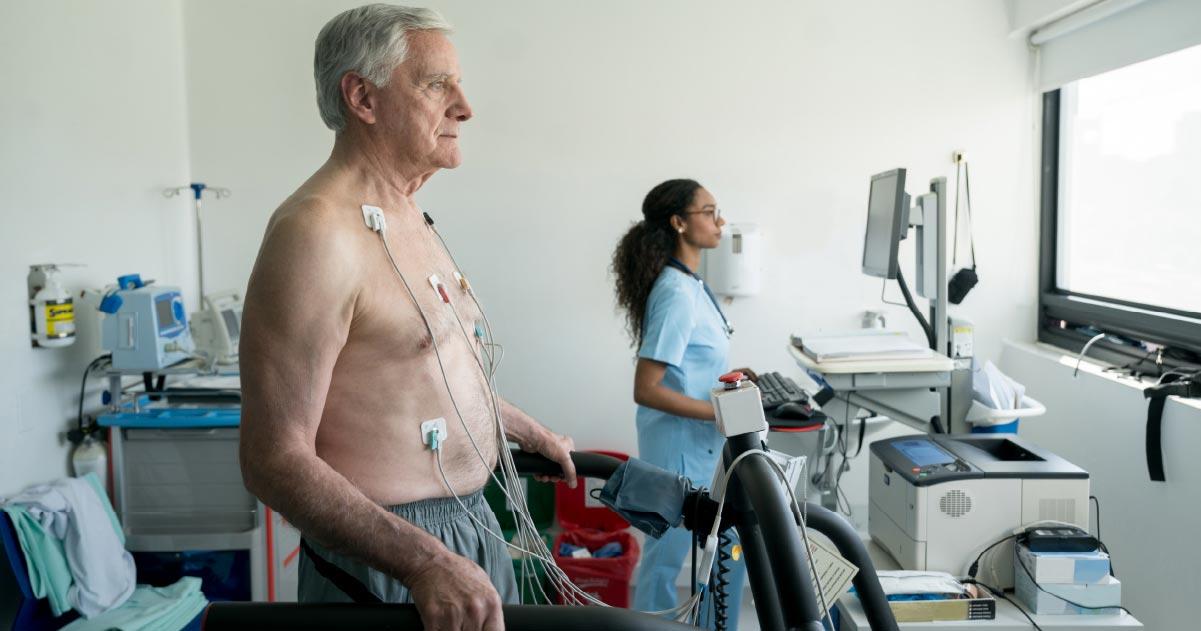
How does a pulse oximeter work?
Unlike an ABG blood test, pulse oximeters are non-invasive and painless.
There are several different types of pulse oximeter (more on this below), but they all work the same way: by sending small beams of infrared light through your skin and into tiny vessels called capillaries.2,4 These light beams bounce off the hemoglobin in your blood and—based on whether the molecules absorb or reflect the light—can determine your blood oxygen level. You’ll see your results on the pulse oximeter’s screen or display.
Why should I use a pulse oximeter?
Using a pulse oximeter to check your O2 saturation can be a helpful way to monitor your health at home.
At the height of the COVID-19 pandemic, for example, many people bought one to keep tabs on their lung function in case they caught the virus. But there are many other situations where you might want to use a pulse oximeter, too. These include:
If you have certain health conditions like:
- Anemia
- Asthma
- Cardiovascular (heart) disease
- COPD
- Lung cancer
- Sleep apnea
If you are taking certain prescription drugs that impact oxygen levels like:
- Medications to treat lung disease
- Opioids
If you want to:
- Identify your own personal baseline O2 saturation
- Measure improvement in your cardiovascular fitness
Types of pulse oximeters
There are prescription and non-prescription pulse oximeters. Many medical supply companies, some online retailers, and device manufacturers themselves offer prescription versions. Non-prescription models are widely available over-the-counter online and in-store.
The U.S. Food and Drug Administration (FDA) tests and approves prescription pulse oximeters intended for medical use and decision-making. Currently, the agency does not regulate non-prescription models for this purpose, though that may soon change.
If you need to check your O2 saturation to monitor a health condition, it makes sense to ask your doctor which type of pulse oximeter to use.
Within each category, common options include:
- Clip-on devices: These pulse oximeters easily attach to your fingertip, earlobe, or toe and can deliver results within a few seconds.
- Medical alert watches: Some of the best medical alert watches include built-in pulse oximeter capabilities. This isn’t a standard feature, however, so it’s imperative to shop around.
- Other wearables: Many health and fitness trackers—like smartwatches, wristbands, and rings—also can measure and monitor your blood oxygen levels during the day and while you sleep.
- Smartphone enabled: These apps use your phone’s camera to shoot infrared beams through your finger to measure blood oxygen.
Keep in mind that accuracy can vary among these categories. Prescription pulse oximeters will always deliver the most accurate blood oxygen readings. Even then, your skin tone can skew results.2,4
Why? It comes down to melanin—the natural pigment that influences your skin, eye, and hair color. Like oxygen-rich hemoglobin, melanin absorbs more infrared light than it reflects.
The darker your skin, the more melanin you have—and the more your skin will absorb infrared light. This can “trick” a pulse oximeter into registering a higher O2 saturation than you have.
How do I use a pulse oximeter?
Once you know how to do it, it’s pretty straightforward to check your blood oxygen level at home. Still, it depends on the type of pulse oximeter you use—so it’s important to read the specific instructions that come with your brand and model.
Basic guidelines include:1,3,4
- Turning off any bright lights in the room
- Sitting or lying in a relaxed position
- Remaining as still as possible during the test
- Keeping your device on for the recommended amount of time
- Removing (or turning off) your device once your oxygen level registers
If you are using a clip-on device or smartphone app to measure through your finger, also be sure to:1,3,4
- Take off any nail polish
- Remove any jewelry from your finger
- Keep your hand below heart level
How do I read a pulse oximeter?
Depending on the type of pulse oximeter you use to check O2 saturation, your results will appear on its built-in screen, on your smartwatch display, or within an app. These results show as a percentage and generally indicate the following:
- 95%–100%: normal range
- 90%–94%: mild hypoxia
- 80%–89%: moderate hypoxia
- Below 80%: severe hypoxia
What factors can affect my readings?
In addition to your skin tone, several other factors can skew your results. These include1:
- Being at higher altitudes
- Having poor blood circulation
- Smoking or vaping
- Wearing nail polish
FAQ
Why do I need to have my blood oxygen level tested?
Your doctor may want to check your oxygen level if you have a medical condition like asthma, cardiovascular disease, COPD, or sleep apnea—or if you take certain medications for lung disease or pain. You can use a pulse oximeter to check your O2 saturation at home, which can help you and your doctor manage your health.
When should I call my doctor?
If you experience any of the symptoms listed in the above article, your healthcare provider can help you identify the cause. Many of these can point to conditions other than hypoxia. If you use a pulse oximeter and it registers a blood oxygen level below 90%, it’s important to call your doctor or visit an urgent care clinic right away.
Does my skin tone affect pulse oximeter readings?
Yes, it can. People with more melanin (darker skin) absorb more infrared light than lighter-skinned people. Because pulse oximeters use infrared light to check blood oxygen levels—and oxygen-rich hemoglobin absorbs this light—this can lead to falsely high results if you’re Black or brown.
Will my insurance pay for a pulse oximeter?
Maybe. In very specific instances, these devices qualify as durable medical equipment (DME) covered by Medicare and other plans. This coverage depends on the state you live in, the health plan you’re enrolled in, and whether your health care provider certifies that the pulse oximeter is medically necessary for your care.
Sources
1. MedlinePlus. Pulse Oximetry. September 12, 2024. Found on the internet at https://medlineplus.gov/lab-tests/pulse-oximetry/
2. Charles Patrick Davis, MD, PhD et al. Hypoxia (Hypoxemia). MedicineNet. May 1, 2024. Found on the internet at https://www.medicinenet.com/hypoxia_and_hypoxemia/article.htm
3. Cleveland Clinic. Blood Oxygen Level. February 8, 2022. Found on the internet at https://my.clevelandclinic.org/health/diagnostics/22447-blood-oxygen-level
4. Ana Gotter. How to Use a Pulse Oximeter. Healthline. September 23, 2024. Found on the internet at https://www.healthline.com/health/pulse-oximetry