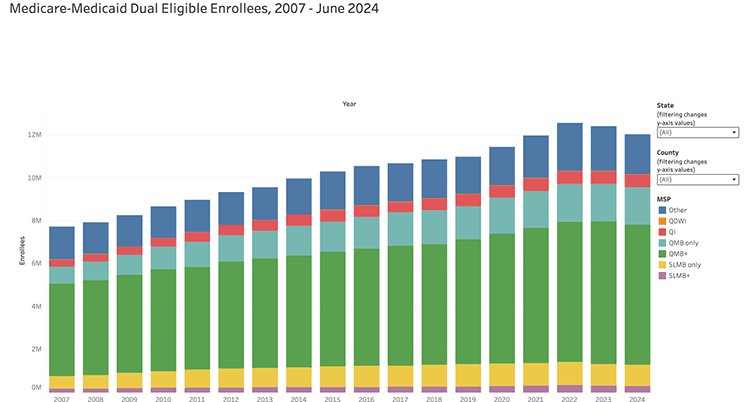
The Medicare-Medicaid Coordination Office at the Centers for Medicare & Medicaid Services (CMS) periodically releases updates to enrollment data for dual-eligible Medicare and Medicaid beneficiaries; the most recent update reflects the period from December 2007 through June 2023.
The visualization below enables you to view enrollment in each dual-eligible (Medicaid and Medicare Savings Programs) program at the state and county level. To view national data, select (All) for State and (All) for County. To see state-level data, select your State and choose (All) for County. County-level data can be viewed by selecting your state and then your county from the list. The enrollment figures are from December of each year. A glossary is available below the visualization. Click here or on the image below to access the table.
The definitions of terms used in this table come from CMS/Medicaid.
QMB (Qualified Medicare Beneficiary): An individual entitled to Medicare Part A, with an income of 100% of the federal poverty level (FPL) or less and resources that do not exceed twice the limit for Supplemental Security Income (SSI) eligibility, and who is not otherwise eligible for full Medicaid benefits through the state. Medicaid pays their Medicare Part A premiums, if any, Medicare Part B premiums, and Medicare deductibles and coinsurance for Medicare services provided by Medicare providers to the extent consistent with the Medicaid State Plan.
QMB+: An individual who meets the standards for QMB eligibility, and who also meets the criteria for full Medicaid benefits. Medicaid pays their Medicare Part A premiums, if any, Medicare Part B premiums, Medicare deductibles and coinsurance, and provides full Medicaid benefits to the extent consistent with the State Plan. These individuals often qualify for full Medicaid benefits by meeting medically needy standards, or by spending down excess income to the medically needy level.
SLMB (Specified Low-Income Medicare Beneficiary): An individual entitled to Medicare Part A, with an income that exceeds 100% FPL but is less than 120% FPL, with resources that do not exceed twice the SSI limit, and who is not otherwise eligible for Medicaid. These individuals are eligible for Medicaid payment of the Medicare Part B premium only. They do not qualify for any additional Medicaid benefits.
SLMB+: An individual who meets the standards for SLMB eligibility, and who also meets the criteria for full state Medicaid benefits. These individuals are entitled to payment of the Medicare Part B premium, in addition to full state Medicaid benefits. These individuals often qualify for Medicaid by meeting medically needy standards or by spending down excess income to the medically needy level.
QI (Qualifying Individual): An individual entitled to Medicare Part A, with an income at least 120% FPL but less than 135% FPL, and resources that do not exceed twice the SSI limit, and who is not otherwise eligible for Medicaid benefits. This individual is eligible for Medicaid payment of the Medicare Part B premium. Prior to FY 2016, the QI program was block granted to states and subject to annual legislative renewal, but it is now permanent as a result of the Medicare Access and CHIP Reauthorization Act of 2015.
Other: An individual who does not meet the income or resource criteria for a Medicare Savings Program, but is eligible for Medicaid either categorically or through optional coverage groups based on medically needy status, special income levels for institutionalized individuals, or home and community-based waivers. *Note that eligibility requirements may differ in some states that have exercised policy options to streamline their MSP eligibility thresholds. For instance, Connecticut and Maine have higher income thresholds for each Medicare Savings Program. In some states, such as California, MSP eligibility requirements may also be fully aligned with Medicaid eligibility, so nearly every MSP enrollee is also enrolled in Medicaid.