Related Topics
Breathing is something we don’t think about too much—until it becomes difficult. For older adults living with chronic lung conditions or other health concerns, getting enough oxygen can feel like a daily struggle. That’s where supplemental oxygen therapy comes in.
Read on to find out what oxygen therapy is, who needs it, and the different modes of delivery. By getting the facts, you’ll know just what to expect, whether you’re exploring oxygen therapy for yourself or someone you care about.
What is oxygen therapy?
Oxygen therapy is a medical treatment that provides extra oxygen to people who aren’t getting enough on their own. According to the National Institutes of Health, more than 1.5 million older adults use supplemental oxygen for a wide variety of health conditions.1
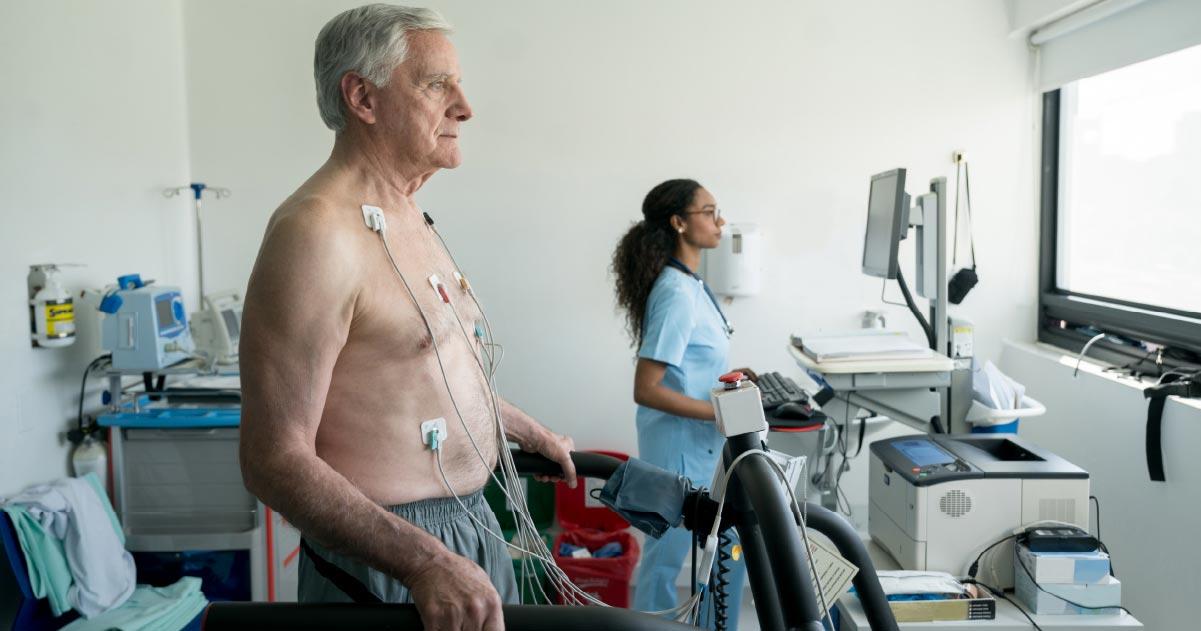
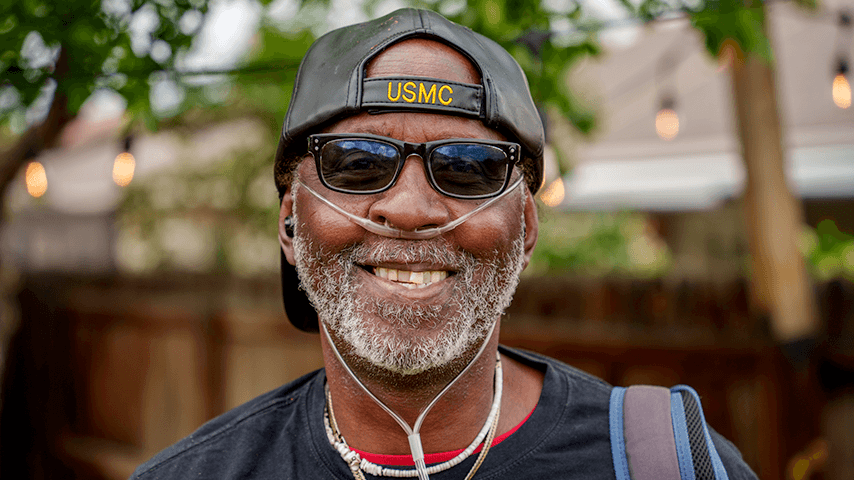
With oxygen therapy, oxygen is supplied through a device such as a nasal cannula (small tubes that rest in your nostrils) or a mask. It may also be delivered through a tent—or a canopy placed over the head and shoulders or the entire body. This delivery system is more common with pediatric patients.
Oxygen therapy is prescribed by a doctor and tailored to each person’s needs.
Who needs supplemental oxygen therapy?
While the air we breathe contains about 21% oxygen, certain health conditions make it harder for the lungs to absorb and deliver enough oxygen to the bloodstream. Supplemental oxygen therapy is most often used for people with chronic lung diseases. It can also help those with heart conditions or other health problems that affect oxygen levels.
Some conditions that may require oxygen therapy include:
- Chronic obstructive pulmonary disease (COPD)
- Emphysema
- Cystic fibrosis
- Chronic bronchitis
- Severe asthma
- Pulmonary fibrosis (lung scarring)
- Congestive heart failure
- Pneumonia (in severe cases)
- Sleep apnea or other sleep-related breathing disorders
How do doctors know if you need oxygen therapy? They may perform tests such as pulse oximetry (a small device that clips onto your finger) or arterial blood gas tests to see if your oxygen levels are abnormally low. A normal oxygen level is usually 95% or higher. If your levels dip below 88%, you may be prescribed oxygen therapy to help you breathe better.
It’s common to use oxygen therapy in the hospital, but it can also be provided at home.
Oxygen therapy for COPD
COPD is one of the most common reasons older adults use oxygen therapy. This long-term lung disease makes it harder to move air in and out of the lungs, leading to low oxygen levels. Supplemental oxygen can help reduce breathlessness and improve energy in people with COPD. It can also lower the risk of complications.
Oxygen therapy for emphysema
Emphysema is a chronic lung disease that damages lung tissue and the air sacs in the lungs, making it difficult for oxygen to pass into the bloodstream. Oxygen therapy can improve a person’s quality of life by easing symptoms and slowing the progression of complications.
What does oxygen therapy do?
At its core, oxygen therapy helps restore normal oxygen levels in the body. This can help:
- Ease shortness of breath and fatigue
- Reduce confusion and increase alertness
- Improve sleep quality
- Support brain and heart function
- Boost energy levels
Types of oxygen therapy
There are several types of systems that deliver oxygen therapy; some are stationary, while others are portable to allow for more mobility. Below are four common methods of delivery.
- Oxygen concentrator. An oxygen concentrator is one of the most popular devices for home use. It works by pulling in room air, filtering out nitrogen, and delivering concentrated oxygen through a tube. Concentrators can run on electricity and provide a steady supply of oxygen as long as they’re plugged in or charged. Portable versions are also available for use outside the home.
- Liquid oxygen. Liquid oxygen is oxygen stored at very cold temperatures in liquid form. It takes up less space than gas, so tanks can be smaller and lighter, which makes them convenient to carry. Liquid oxygen systems can be helpful for people who want to be able to move around more easily with their equipment.
- Compressed gas cylinders. These are traditional oxygen tanks filled with compressed oxygen gas. They come in different sizes, from large tanks for home use to small portable ones. But these tanks need regular refilling and can be heavy to move around.
- Portable oxygen concentrators (POCs). POCs are lightweight, battery-powered devices that are a good fit for people with active lifestyles (many are even approved for airplanes!).
Oxygen therapy cost
The cost of home oxygen equipment can vary quite a bit depending on the type of equipment, how often you use it, and whether insurance helps cover it:
- Monthly rental costs of a portable oxygen device start around $150.
- Portable oxygen concentrators generally range from $1,000-$2,500 for used equipment and $2,000-$4,000 for new equipment. Battery life, oxygen output, and weight are some of the factors that affect cost.
- Refills for tanks and maintenance services may add to ongoing costs.
Does Medicare cover oxygen therapy?
Yes. Oxygen therapy is covered under Medicare Part B if your doctor prescribes it for use at home. But instead of buying the equipment outright, Medicare pays the supplier a monthly rental fee for up to 36 months. This fee covers the equipment, accessories, and any oxygen-related services you need.
After the 36 months are up, the supplier must keep providing your oxygen equipment and services for up to five years, as long as your doctor confirms you still need it. You’ll still be responsible for your Part B deductible and 20% coinsurance. For more information, see our guide: Will Medicare Cover Durable Medical Equipment?
Many private insurance plans also cover part of the cost of oxygen therapy that’s considered medically necessary, but it’s important to check your coverage with your carrier.
Is oxygen therapy safe?
When used as prescribed, oxygen therapy offers many benefits, including better quality of life, fewer hospital visits, and reduced risk of serious complications from low oxygen levels. But there are some things to consider before starting therapy, including side effects and safety.
Side effects of oxygen therapy
Possible side effects of oxygen therapy include dryness in the nose or throat, nosebleeds, headaches (especially in the morning), and skin irritation where the tubing rests. Some people may also experience fatigue. These side effects can usually be managed with small adjustments or the addition of a humidifier to the home.
Safety tips for oxygen therapy
Oxygen on its own is not flammable. But it can intensify the combustion of other materials. To reduce the risk of injury:
- Do not smoke or let anyone smoke near oxygen equipment.
- Keep oxygen away from open flames or gas stoves.
- Store tanks securely so they don’t tip over.
- Use only the equipment provided by your supplier—never try to fix or modify it yourself.
How often do you need oxygen therapy?
The frequency of oxygen therapy depends on your health needs. Some people may only require it during sleep or activity, while others need it around the clock.
How much oxygen do you need?
If your doctor prescribes oxygen therapy, they’ll set a specific flow rate, such as 2 liters per minute (LPM). This means 2 liters of oxygen are delivered through your nasal cannula each minute. Most prescriptions range from 1 to 10 LPM, with most patients—about 70%—needing 2 liters or less.
Oxygen can be delivered via two methods, continuous and pulse:
- Continuous flow: With this delivery method, oxygen flows steadily, even when you’re not inhaling.
- Pulse flow: With pulse flow, oxygen is delivered in bursts when you inhale (using a sensor that detects your breath). This method helps conserve supply.
Your doctor or respiratory therapist can help you determine whether you need a pulse or continuous flow unit. The right system for you depends on your medical needs, your personal preferences, and often, your daily activity level.
Will you always need to use oxygen therapy?
Some people may only need oxygen therapy temporarily—for example, while recovering from pneumonia. Others, especially older adults with chronic disease affecting the lungs, may need it long-term.
Frequently asked questions (FAQ)
Is oxygen therapy a treatment for pneumonia?
Yes. While it does not treat the infection itself, oxygen therapy can play an important role in treating severe cases of pneumonia. It’s used temporarily to boost blood oxygen levels and reduce strain on the lungs and heart, which helps prevent organ failure and other major complications. Oxygen therapy also helps relieve symptoms like shortness of breath and fatigue.
What happens if you use oxygen therapy and don’t need it?
Using oxygen when you don’t need it won’t provide any health benefit. In fact, if your oxygen levels aren’t low, supplementing with too much oxygen could dangerously slow your heart rate and breathing.
What is hyperbaric oxygen therapy?
Hyperbaric oxygen therapy is a specialized treatment where patients breathe pure oxygen in a pressurized chamber. It’s used for conditions like carbon monoxide poisoning or decompression sickness, not for COPD or emphysema.
Do you need to use oxygen therapy when sleeping?
Some people only have low oxygen levels during sleep, so their doctor may prescribe nighttime oxygen therapy. If there’s a concern about your oxygen saturation levels while sleeping, your provider can order an overnight oximetry test.
Sources
1. National Heart, Lung, and Blood Institute. NHLBI Air You Wear Challenge. Updated April 3, 2023. Found on the internet at https://www.nhlbi.nih.gov/grants-and-training/air-you-wear-challenge
2. Chiagozie Nwasuruba, MD, FACP, SFHM, FABQAURP, et al. Long-term supplemental oxygen therapy. UpToDate. Feb. 13, 2025. Found on the internet at https://www.uptodate.com/contents/long-term-supplemental-oxygen-therapy/print