A traumatic brain injury (TBI) is a potentially life-changing event. It can affect our ability to do all those things we take for granted—like solving problems, focusing on a task, making decisions, and even speaking and walking. People who suffer a TBI, including older adults, are also at greater risk for developing mental health disorders.
During a session at our Older Adults Mental Health Awareness Day (OAMHAD) Symposium, called "Traumatic Brain Injury and Mental Illness Among Older Adults,” a panel of experts explored the key causes of TBIs in older adults and their impact on mental health.
What is a traumatic brain injury?
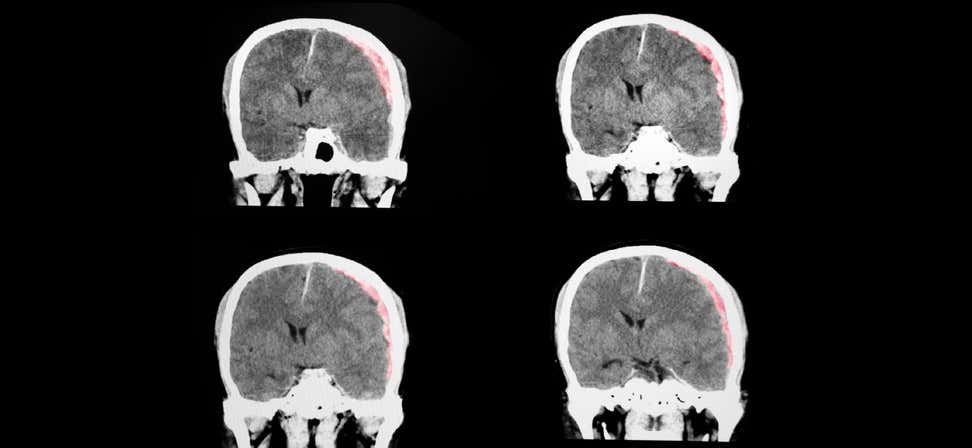
A traumatic brain injury is a type of injury that occurs when a sudden, external force or trauma affects the brain’s functioning. This force can result from a blow or jolt to the head (closed brain injury) or penetration of the skull (penetrating brain injury). "You may bump your head and it may hurt, but that doesn't necessarily mean that there's been a brain injury," said OAMHAD presenter Michael Hall, PhD, LCP, an Associate Professor in the Department of Physical Medicine and Rehabilitation at Virginia Commonwealth University. “There really needs to be disruption of how the brain is working."
While TBIs can happen to people of all ages, older adults are especially vulnerable. In fact, people age 75 and older have the highest rates of TBI-related hospitalizations (32%) and deaths (28%).1
What are the symptoms of a traumatic brain injury (TBI) in older adults?
TBIs are typically categorized as mild, moderate, or severe, based on the degree of impact on brain functioning. A brain injury may or may not involve a loss of consciousness immediately after the traumatic event. Symptoms of a mild TBI include:
- Confusion
- Memory issues
- Trouble speaking clearly
- Headache
- Dizziness
- Nausea and vomiting
- Sensitivity to light and/or sound
- Ringing in the ears
What is the most common cause of TBI in older adults?
Falls are the leading cause of traumatic brain injury, accounting for nearly half of all TBI-related hospitalizations. Older adults are at high risk, with more than 1 in 4 people age 65+ falling each year.2
“The most common cause of traumatic brain injuries in the elderly are falls, and falls can be due to multiple issues,” explained Hall. “It can be just a trip, or medical issues such as cardiac problems or syncope (fainting or passing out). There are movement problems that can result in people falling as well as medication issues, things like benzodiazepines that can sedate and increase your fall risk.”
Motor vehicle accidents are a frequent cause of TBI in older adults age 60 to 75. Other reasons for traumatic brain injury include firearm-related suicide attempts, assaults, and being struck by or against an object.
Does age matter in brain injury recovery?
Older age is a known risk factor for poorer prognosis after a TBI. One reason for this, Hall explained, is normal age-related changes and decreased brain plasticity as we get older. Older adults tend to have:
- A higher risk for brain bleeds
- Slower recovery rates
- Higher level-of-care needs
- A greater likelihood of existing medical/mental health issues that worsen functioning
- A higher risk for mild cognitive impairment, dementia, and other neurological disorders
How does traumatic brain injury affect mental health?
While most TBIs are non-life-threatening, they can still have long-lasting physical, cognitive, behavioral, and emotional effects for older adults. A 2019 study found that roughly 1 in 5 people may experience TBI mental health symptoms up to six months after a mild traumatic brain injury.3 Major depression is the most common mental health diagnosis,4 followed by:
- Anxiety disorders
- Post-traumatic stress disorder (PTSD)
- Irritability, anger, emotional lability
- Adjustment disorder
- Substance misuse or abuse
- Psychosis and mania
- Personality changes
People suffering a TBI also have higher-than-normal rates of non-fatal self-harm and suicide.5
Certain predisposing factors can make it more likely for an older adult to experience mental health troubles after a TBI. These include sleep problems, anxiety, alcohol and/or drug use, low income, negative thinking, and poor social functioning. In addition, a brain injury can increase the symptoms of a pre-existing mental health disorder.
In the year following a traumatic brain injury, secondary factors can complicate mental health conditions, such as loss of employment, inability to drive, sleep issues, relationship problems, and social isolation.
What is the treatment for mental health issues after TBI?
Hall said that since mental health issues typically arise within six months after a TBI, early intervention is critical. A good place to start is with an in-depth neuropsychological assessment to identify TBI mental health symptoms and create a tailored treatment plan. “And that means collaborative teamwork,” he said. “Rehabilitation is a team sport.” Elements of a traumatic brain injury mental health treatment plan may include:
- Screenings (cognitive, mood, suicidality)
- Referrals to mental health resources (e.g., therapy, medication management, substance abuse counseling)
- Symptom management / disease management
- Tracking (cognitive, mood, functioning)
- Assessment of barriers to care
- Crisis and safety planning
- Social/family/peer support
- Referrals to social workers and/or nurse case managers
Practicing healthy behaviors is another vital part of managing mental health conditions and other TBI-related symptoms. These include:
- Regular exercise
- A healthy, plant-based diet
- Good sleep habits
In addition, stress management techniques can help older adults better control their TBI mental health symptoms. OAMHAD presenter Ken Collins, a TBI advocate and Executive Director of the Hozho Center for Personal Enhancement, explained how relaxation techniques help him manage his own TBI symptoms. “I'm a lot more prepared to get older with these memory issues because of all of the strategies that I've gained to be able to make it through my days,” said Collins, who is 72 and has been living with a brain injury for 46 years.
Universal strategies for coping with a TBI
People with brain injuries tend to experience the world differently than they did before, and accommodations may be required to help them adapt. "It is good to be informed whether you're the provider, you're the individual with a brain injury, or you're a family member," said OAMHAD presenter Maria Crowley, MA, CRC, Director of Professional Development at the National Association of State Head Injury Administrators (NASHIA). She shared simple strategies for managing TBI-related challenges, such as:
- Keep noise and light to a minimum whenever possible
- Limit distractions and work on one task at a time
- Provide written direction whenever possible
- Break large amounts of information into smaller "chunks" or steps
- Don't mistake lack of emotion for lack of interest
- Provide neutral, but direct, feedback
- Be factual; avoid abstract concepts
- Prioritize and organize tasks to be performed
The importance of TBI screening for older adults
Brain injuries are considered a "silent epidemic," meaning they aren't always easily recognized. Someone with a TBI can appear perfectly normal on the outside. This is one of the reasons TBIs so frequently go undiagnosed, misdiagnosed, or mistreated. If you suspect you have a brain injury, don’t ignore it. Talk to your health care provider about a TBI screening.
Reduce your TBI risk by taking steps to avoid falls
Since most traumatic brain injuries are caused by falls, you can reduce your risk by practicing these basic falls prevention techniques:
- Get your vision and hearing checked: Annual exams can help you make sure you're in tune with the environment around you.
- Use assistive devices if needed: A device like a walker can provide extra support if you have poor balance, muscle weakness, or other mobility problems.
- Regularly review your medications: Ask your doctor or pharmacist to identify any potential side effects that can increase your falls risk.
- Fall-proof your home: Stay safe by removing tripping hazards, installing grab bars in bathrooms and stairways, removing loose rugs, and making sure lighting is sufficient throughout your residence.
- Find a balance and exercise program: Call your local area agency on aging to see what programs are available in your area.
- Talk to your family: It takes a village to prevent falls! Ask for your family members’ support in maintaining a "falls free" lifestyle.
- Take a falls risk assessment: Check your risk for falling with our Falls Free CheckUp and share your score with your health care provider.
For more falls prevention tips and resources, visit our Falls Prevention for Older Adults resource library.
Sources
1. Centers for Disease Control and Prevention (CDC). Traumatic Brain Injury & Concussion. Found on the internet at https://www.cdc.gov/traumaticbraininjury/data/index.html
2. Centers for Disease Control and Prevention (CDC). Facts About Falls. Found on the internet at https://www.cdc.gov/falls/facts.html
3. National Institutes of Health. Mental health disorders common following mild head injury. January 30, 2019. Found on the internet at https://www.nih.gov/news-events/news-releases/mental-health-disorders-common-following-mild-head-injury
4. Marcelo Schwarzbold et al. Psychiatric disorders and traumatic brain injury. Neuropsychiatric Disease and Treatment. August 2008. Found on the internet at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2536546/
5. Yueh-Chien Lu et al. Association between suicide risk and traumatic brain injury in adults: a population based cohort study. Postgraduate Medical Journal. February 3, 2020. Found on the internet at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7788485/
This project was supported, in part by grant number 90CSSG0048 and 90FPSG0051 from the U.S. Administration for Community Living, Department of Health and Human Services, Washington, D.C. 20201. Grantees undertaking projects under government sponsorship are encouraged to express freely their findings and conclusions. Points of view or opinions do not, therefore, necessarily represent official Administration for Community Living policy.