Millions of Americans live with some form of heart disease right now—including the vast majority of Medicare recipients.
Also known as cardiovascular disease (CVD), heart disease can lead to heart attack, stroke, heart failure, and other negative health outcomes. As a result, according to the most recent statistics released by the American Heart Association, CVD is the leading cause of death in the United States for people across nearly all racial and ethnic groups.
“That may sound like bad news, but it doesn’t have to be,” explained Jennifer Tripken, associate director of NCOA’s Center for Healthy Aging. “There are steps you can take to protect the heart health you have, even if it’s too late to prevent cardiovascular disease entirely.”
For certain people, those steps include cardiac rehabilitation therapy—a medically supervised program designed to help patients reduce their risks and improve their quality of life through physical activity, lifestyle modifications, and counseling.
Cardiac rehab is commonly recommended for patients after:
- Suffering a heart attack
- Getting a stent
- Undergoing bypass surgery
- Experiencing heart failure
- Having certain other heart-related procedures
But you don’t have to wait for any of these things to happen either, says Tripken. “Don’t let the word ‘rehabilitation’ fool you into thinking this program is only for people who have suffered serious cardiac events.”
Proactive participation can benefit nearly everyone who lives with heart disease, even if it’s well controlled,” Tripken said.
And yet, fewer than 20 percent of eligible patients actually follow through, according to the American Heart Association.1 This includes many older adults who may feel limited by their age, additional health issues, or other barriers.
You don’t have to be one of them. “Cardiac rehab specialists are trained to tailor the program according to their patients’ age and physical capacity,” Tripken explained. “If your health care provider has suggested cardiac rehab, you owe it to yourself to at least explore the possibility.”
Do you wonder if a cardiac rehabilitation program is right for you or someone you love? Find answers to common questions below.
What exactly is cardiac rehabilitation therapy?
The major goal of any cardiac rehab program is to improve the way a patient’s heart functions so they may:
- Reduce their risk for heart attack and other adverse events
- Limit the negative effects of physical and psychological stress
- Enjoy a better quality of life
In order to do this, a coordinated team of health care providers, nutritionists, exercise specialists, and counselors works with each patient to design a comprehensive plan that addresses individual risk factors. These might include:
- High blood pressure
- Obesity
- Diabetes
- Inactivity
- Smoking
- Stress
During cardiac rehab, participants learn how to make heart-healthy choices as well as positive changes to their lifestyle and habits. Often, they also benefit from the support and positive reinforcement of others who are going through the program.
What are the main parts of cardiac rehabilitation?
Generally speaking, cardiac rehab includes three phases:
1. Inpatient (3-7 days)
Patients who have been hospitalized for a heart-related condition or surgery may begin cardiac rehab at the bedside. Keeping in mind that every patient’s needs and capacities will be different, Phase I may include very gentle exercise—led and monitored by nurses or other trained medical professionals—as well as education on how to manage stress.
2. Outpatient (12 weeks)
Anyone with heart disease—whether they were previously hospitalized or not—can participate in Phase II cardiac rehabilitation as long as their cardiologist approves it and they feel ready.
During this phase, a special community-based rehabilitation team assesses the patient, taking into account things like their:
- Specific heart condition
- Current capacity for exercise
- Physical limitations (if any)
- Other medical conditions (if any)
- Individual risk factors
- Goals
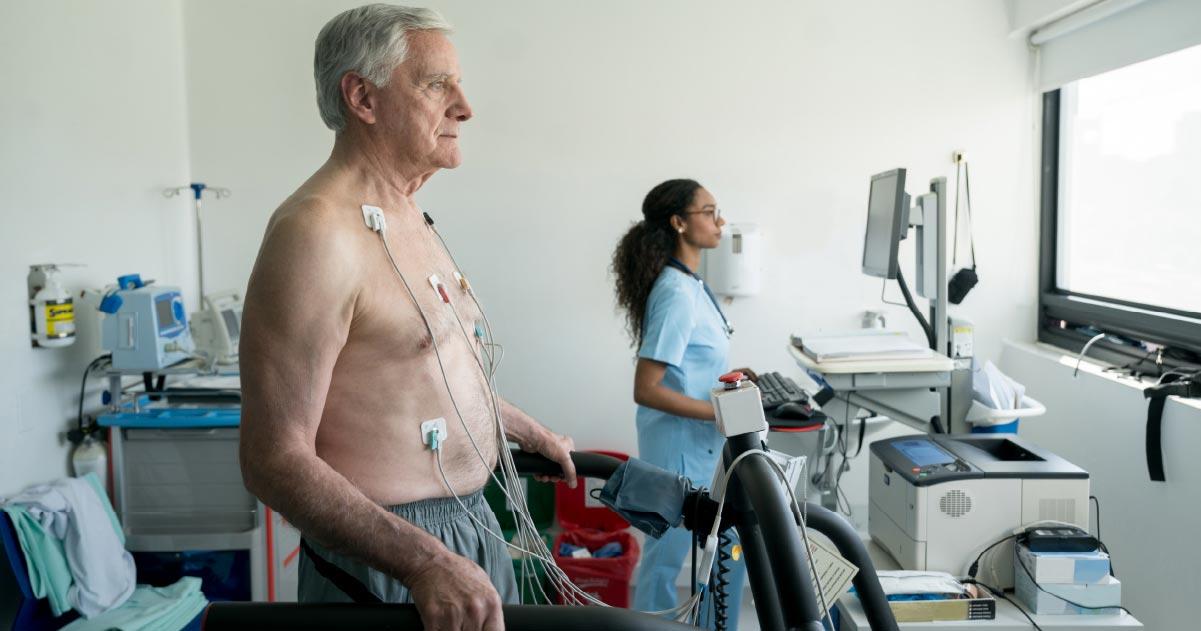
Then, the team partners with the patient to design an individualized therapy program that includes monitored physical activity (such as walking on a treadmill); stress reduction strategies (such as mindfulness and meditation); and lifestyle interventions (such as nutritional counseling or smoking cessation classes). Cardiac rehab specialists guide the patient at every step to ensure a medically safe environment and to support healthy progression.
Depending on the patient, Phase II generally includes 2-3 sessions per week for up to 12 weeks.
3. Independent maintenance (ongoing)
Phase III boils down to one word: follow-through.
Once a patient “graduates” from Phase II cardiac rehab, it’s time to apply what they learn to daily life. This means finding the motivation to continue exercising safely, stick to a healthy diet, and manage risk factors. But they don’t have to do it alone. Many programs include ongoing support to help keep patients on track.
What is the difference between cardiac rehab and physical therapy?
Actually, there is some overlap.
Physical therapy helps a person increase their strength, balance, flexibility, and mobility through activities such as walking, cycling, weight training, stretching, yoga, and more. Cardiac rehabilitation therapy helps patients improve their heart function through a more comprehensive approach that includes—but isn’t limited to—some form of physical therapy.
For example, patients enrolled in cardiac rehab may ride a stationary bike or learn gentle stretches to help their chest muscles recover from surgery. But their sessions don’t end there, as noted above.
What are the benefits of cardiac rehab?
Cardiac rehabilitation helps the heart recover from injury, surgery, or disease. It also helps participants:
- Lower their risk factors for future heart attacks
- Regain strength and mobility
- Form healthier habits
- Manage the anxiety of living with heart disease
- Prolong their life
I’m interested. Where can I find a cardiac rehabilitation program?
You will need a referral, so be sure to talk to your cardiologist or other health care provider about options near you. In many cases, Medicare will cover the costs; be sure to ask about that, too.
Source
1. The American Heart Association, “Cardiac Rehab: Frequently Asked Questions.” Found on the internet at https://www.heart.org/en/health-topics/cardiac-rehab/cardiac-rehab-faq.