Key Takeaways
Access to factual, clear, and culturally responsive information about Medicare is needed now more than ever. By 2025, racial and ethnic minority older adults will more than double and will account for more than one in three Americans 65+.
NCOA reaffirmed its commitment to women, low-income, communities of color, the LGBTQ, and rural older adults in our Equity Promise.
Factors like socioeconomic and health status – exacerbated by the pandemic – demonstrated how policies applied unequally have devastating affects over a person’s lifetime.
On Medicare’s historic 56th birthday, we must celebrate the decades of protection, better health, and well-being of older Americans, and how the program has increased the financial security of our nation.
However, birthdays are as much a time for celebration as they are for reflection on the realities of what we wish for ourselves and those we love in the years ahead.
Every person born in this world will age. By 2030, those aged 65+ will increase from 49 million to 71 million. COVID-19 laid bare the need for our current systems to be improved – with the pandemic’s harsh realities cutting differently across different communities.
Hispanic/Latinx, Indigenous, and Black Americans all have a COVID-19 death rate of double or more that of White Americans. Decades of structural opportunities for some and oppressive policies for others, lack of access to healthcare and services over a lifetime, and other socioeconomic factors put communities of color at a greater risk for not being able to afford health insurance as a younger person, thus impacting the ability to afford any supplemental coverage outside of traditional Medicare on their 65th birthday.
The Affordable Care Act brought dramatic progress to this issue, but coupled with Medicare improvements, it could bring a 20th century designed program to fit our 21st century needs, especially for the most vulnerable today. When we know better, we do better.
Paving the Way - Then
In 1965, Medicare was critical to desegregating hospitals, requiring them to comply with the Civil Rights Act in order to receive payment. At the time, a structural change to existing programs contrasted the de jure and de facto inequalities of our nation’s policies around healthcare, housing, education, transportation, among others – paving the way for greater access for racial and ethnic minorities on Medicare.
Paving the Way - Now
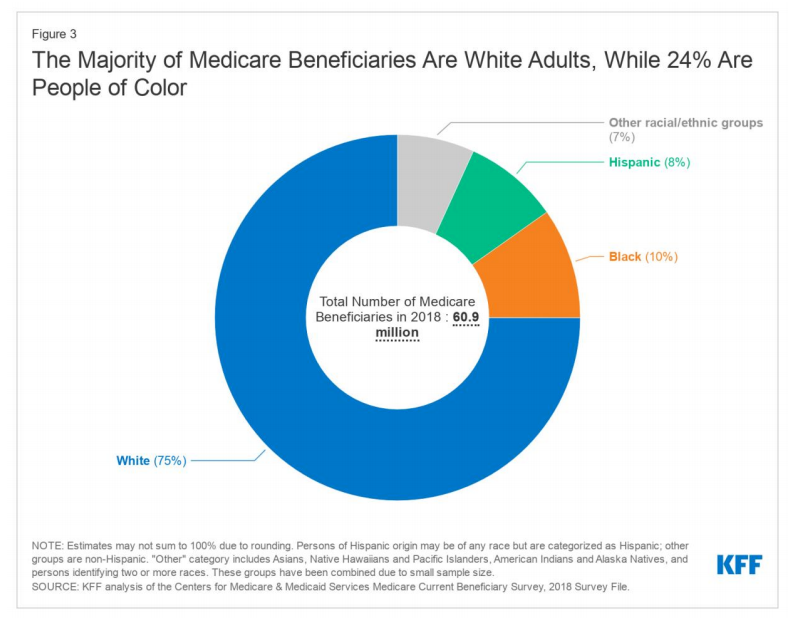
Among Medicare beneficiaries, people of color are more likely to report being in relatively poor health and have higher rates of chronic conditions like hypertension and diabetes than White beneficiaries. They are also less likely to have one or more doctor visits, but have higher rates of hospital admissions and emergency department visits than White beneficiaries.
The Kaiser Family Foundation analyzed patient data from health records showing that in addition to having higher rates of infections, hospitalizations, and mortality, people of color have been more likely to require a more intensive level of treatment at the time of COVID-19 diagnosis, such as inpatient hospitalization or the use of oxygen and ventilation.
Further, the pandemic has exacerbated mental health outcomes among older Hispanic/Latinx adults, who report higher rates of depression or anxiety (33%) than older White (23%), Black (26%), and Asian (17%) adults.
The moral and business case for amplifying the needs of older low-income, ethnic, and racial minorities, the LGBTQ, and those with disabilities was demonstrated through the impact on these specific populations during the pandemic. It shed light on the fact that social determinants of health like transportation and housing are just as critical to the overall health and well-being of these populations as access to a hospital or provider. Factors like these should be taken into consideration when reevaluating the way we measure a system that works for all.
On this 56th Medicare birthday, we must continue to navigate the pandemic by learning from and applying the most effective models of social change. We must celebrate our accomplishments from the last half-century while acting upon the changing demographics that require us to invest, educate, and provide information on improvements to Medicare in the next 50 years.
Everyone’s Invited to Do Better
At NCOA, we look to the legacies of community-centric leaders like Ella Baker, Cesar Chavez, Marsha P. Johnson, and others as we shift the paradigm on equitable aging for years to come. Medicare improvements are no exception to important components of social change. They are critical to its viability.
Working toward equitable aging means that every step with the intention to bring those most at the margins to the center is an important one.
When we know better, we do better, and everyone must be invited to the party.











